Establishing Undeniable Proof to Fight Denials and Win at Community Health Network
KEY INITIATIVES
Document authorization, insurance verification and notification activities – voice, fax and electronic – for proof to prevent and overturn denials.
Convert to paperless workflow with electronic faxing and image export to the EHR.
Centralize insurance exchanges for enterprise access to reduce rework and shorten appeals process.
PROJECT SUMMARY
Community Health Network uses Trace® by Vyne Medical to record phone conversations, send/receive faxes and capture activity from web sites and other hospital systems. All activity is tied to the patient account and centrally stored for enterprise access and exchange.
Denial team receives denial or request for more information
Team checks EHR for reference number to voice recording, fax or image; retrieves record for proof to fight denial
PROOF POINTS
![]() If proof is found in voice recording: Team sends transcript of recorded call showing proof of authorization or agreed-upon level of care.
If proof is found in voice recording: Team sends transcript of recorded call showing proof of authorization or agreed-upon level of care.
![]() If proof is found in fax: Team sends documentation letter showing content of fax and date/time stamp for proof of timely notification or of clinicals being delivered. Denials are routinely overturned using proof of these interactions and there’s no more rework and back-and-forth between departments.
If proof is found in fax: Team sends documentation letter showing content of fax and date/time stamp for proof of timely notification or of clinicals being delivered. Denials are routinely overturned using proof of these interactions and there’s no more rework and back-and-forth between departments.
WORKFLOW | COMMUNICATION | TIME |
ChallengeDisconnect between care management and patient access | ChallengeDisconnect between care management and backend departments | ChallengeTime spent on manual tasks such as printing and scanning
|
ActionCare Management absorbed employees from patient access center and surgery authorization verification team | ActionTrace applications implemented for voice recording, electronic faxing and image capture for Care Management and other departments | ActionCare management implemented Trace electronic faxing and integration tools for automatic export of images to the patient record |
ResultStreamlined workflow and strengthened denial management with additional patient insurance representatives | ResultAuthorization, notification, clinicals and level of care activities are documented, indexed and centrally stored | ResultStreamlined care management workflow and eliminated the need to print, scan and manually fax information
|
PROJECT OUTCOMES
 Time and Cost Savings
Time and Cost Savings
Utilization Review has direct access to information needed to support claims
- Electronic faxing and image export reduce paper and machine costs. Non-clinical staff process faxes and alert appropriate case manager, to reduce administrative burden for RNs
Back-end works accounts faster with fewer manual touches and less rework between departments. Denial management team completes reviews in a more timely manner, leading to earlier discharges and reduced length of stay
IMPACT
Community has responded to increasing demands from payers without increasing FTEs in UR or Denial Management. Initial plans to hire 5 additional RNs became unnecessary because of efficiencies gained with centralized access to care management data. This saved the network the equivalent of 5 FTEs with benefits.

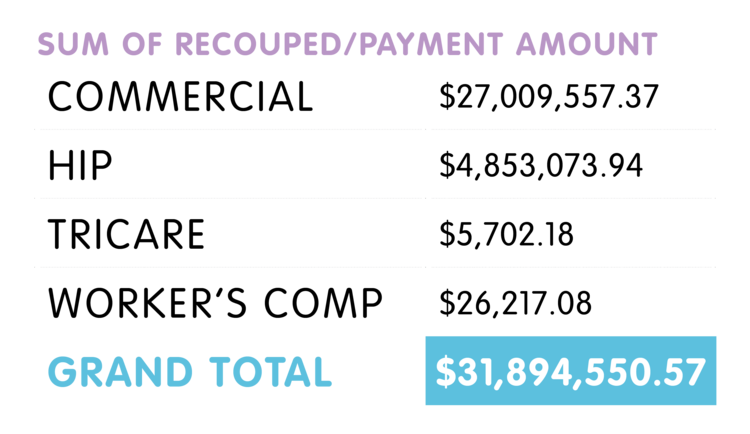
 Time and Cost Savings
Time and Cost Savings